Last Updated on 23/04/2025 by Admin
Comprehensive Insights into Otosclerosis
Defining Otosclerosis: Causes and Mechanisms
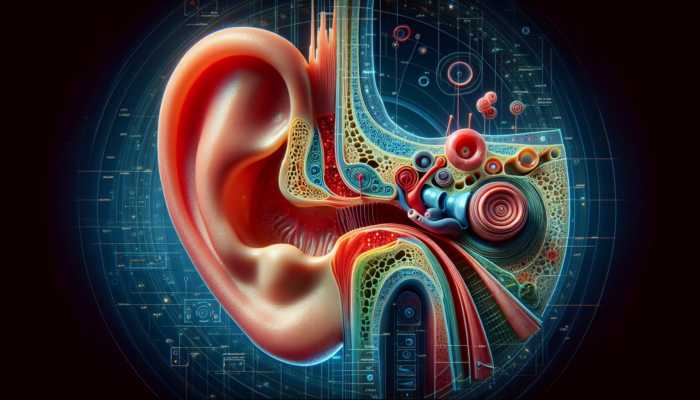
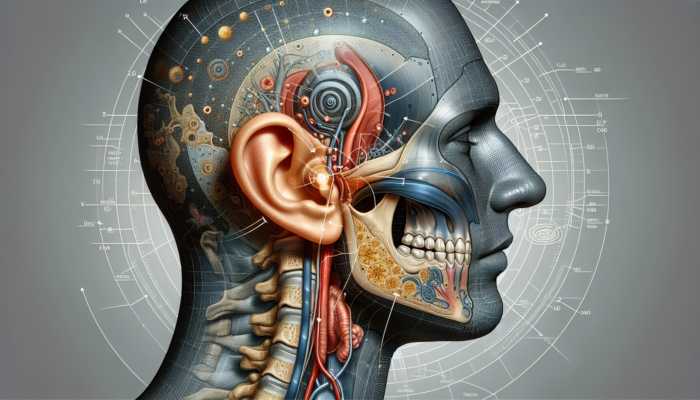
Otosclerosis is a complex medical condition that primarily affects the stapes bone located in the middle ear. This condition impedes the bone’s ability to move freely, resulting in a gradual but significant impact on hearing. The stapes plays a crucial role in the transmission of sound waves from the outer ear to the inner ear. When it becomes fixed due to otosclerosis, this delicate process is interrupted, leading to various auditory challenges. One of the leading contributors to this condition is genetic predisposition; individuals with a family history of otosclerosis have a heightened risk of developing it themselves. The intricate balance of sound wave transmission is disrupted, which can cause a series of auditory difficulties.
The precise causes of otosclerosis are still being explored by medical researchers. While genetic factors are well-established, there is growing evidence that environmental influences might also play a significant role. Some studies have proposed that viral infections could be linked to the onset of otosclerosis, though conclusive causes remain elusive. As a result, individuals diagnosed with otosclerosis often experience uncertainty regarding their condition, highlighting the importance of increased awareness and education about this complex disorder.
Understanding the Prevalence and Demographics of Otosclerosis
When examining the demographics associated with otosclerosis, a clear trend emerges. This condition is most commonly found in adults, particularly those in their 20s and 30s, with a notable prevalence among females. The global prevalence of otosclerosis is estimated to affect approximately 0.3% to 0.4% of the population. If left untreated, this can lead to a considerable number of individuals suffering from varying degrees of hearing impairment.
Interestingly, otosclerosis does not show bias toward geographical locations. Whether in the busy urban landscapes of North America or the serene rural communities in Asia, otosclerosis can arise across diverse demographics worldwide. Understanding these demographic factors is crucial for healthcare providers, as it allows them to tailor their diagnostic and treatment strategies effectively, ensuring resources are directed towards those most susceptible to this condition.
Importance of Early Detection and Accurate Diagnosis of Otosclerosis
Early identification of otosclerosis is essential for effective treatment and management. The first step typically involves comprehensive hearing tests, including audiograms that assess an individual’s ability to perceive different sound frequencies. An extensive review of the patient’s family history can provide vital information that reveals potential hereditary factors influencing the diagnosis.
In certain instances, advanced diagnostic tools like CT scans may be utilized to gain a clearer picture of the middle ear’s structure. These imaging techniques not only confirm the diagnosis of otosclerosis but also help distinguish it from other forms of hearing loss. The significance of timely diagnosis cannot be overstated, as it opens avenues for potential interventions that can greatly enhance an individual’s quality of life.
Exploring Available Treatment Options for Otosclerosis
The array of treatment options for otosclerosis is both varied and evolving. For those experiencing mild to moderate hearing loss, hearing aids can provide a significant benefit by amplifying sound and improving the ability to communicate effectively. These devices are available in numerous styles and technologies, specifically designed to address the unique needs of each user.
For individuals facing more severe cases of otosclerosis, surgical options such as stapedectomy or stapedotomy present promising alternatives. These surgical procedures involve the replacement of the immobilized stapes bone with a prosthetic device, thereby restoring the essential function of sound transmission and enhancing hearing capabilities. While surgical interventions can be highly effective, they also come with inherent risks that must be carefully considered by the patient and their healthcare provider.
In some instances, medical management may involve fluoride therapy, which aims to slow the progression of otosclerosis. Although the efficacy of this treatment remains a subject of debate among medical professionals, it highlights the necessity for a multifaceted approach in managing the condition. Continuous advancements in medical research are vital in shaping effective treatment strategies for otosclerosis.
Identifying Symptoms and Understanding Progression
Recognizing the Initial Symptoms of Otosclerosis
Detecting the initial symptoms of otosclerosis can be quite challenging, as they tend to manifest gradually and subtly over time. The most common early sign is a slow but noticeable decline in hearing, which often goes unrecognized initially. Many individuals may attribute this hearing loss to the natural aging process or the typical noise of daily life, particularly in our increasingly loud environments.
In addition to hearing loss, individuals frequently report experiencing tinnitus, characterized by a ringing or buzzing sensation in the ears. This can complicate the auditory experience further. Some individuals might also experience episodes of vertigo, leading to feelings of dizziness and imbalance. While these symptoms may seem relatively innocuous at first glance, if left unaddressed, they can escalate into more significant concerns, underscoring the necessity for awareness and prompt medical intervention.
Understanding the Progression of Hearing Loss Due to Otosclerosis
The progression of hearing loss associated with otosclerosis exhibits a wide range of variability among individuals. For some, symptoms may begin as mild impairments, while others may experience a swift decline, culminating in profound hearing loss in both ears. The unpredictable nature of this condition can be frustrating, leading to uncertainty in daily interactions and social engagements.
Prompt intervention is critical in managing hearing loss progression. Regular consultations with audiologists can help monitor changes in auditory capabilities and facilitate timely responses to emerging challenges. As awareness and understanding of otosclerosis increase, individuals become better equipped to seek help and implement strategies that may slow the progression of their condition, thus enhancing their quality of life.
Exploring the Impact of Otosclerosis on Daily Life
The challenges posed by otosclerosis can profoundly affect day-to-day living. As communication becomes increasingly difficult, especially in noisy environments or crowded settings, misunderstandings can arise, leading to feelings of frustration and isolation. As the condition progresses, individuals may withdraw from social interactions, fearing a decline in their quality of life due to their hearing difficulties.
The emotional impact of this condition can also be significant. Many individuals struggle with feelings of misunderstanding or exclusion, which can lead to heightened anxiety and self-doubt. Fostering a supportive environment, whether through connections with family and friends or community resources, can help alleviate some of these challenges, promoting a sense of belonging and emotional well-being.
Evaluating Treatment Strategies for Otosclerosis
Harnessing the Benefits of Hearing Aids
Hearing aids represent a beacon of hope for many individuals dealing with mild to moderate hearing loss as a result of otosclerosis. These sophisticated devices function by amplifying sound, allowing users to engage more fully in conversations and everyday activities. With ongoing advancements in technology, modern hearing aids now come equipped with features such as noise cancellation and directional microphones, enhancing their effectiveness in challenging auditory environments.
Customization plays a key role in the effectiveness of hearing aids—each individual’s hearing loss pattern is unique, and devices can be tailored to meet specific requirements. A comprehensive consultation with an experienced audiologist can help determine the most appropriate device, ensuring a comfortable fit and optimal performance. Embracing hearing aids can empower individuals to reclaim their auditory experiences, fostering deeper connections with others and enhancing overall quality of life.
Exploring Surgical Interventions for Severe Cases
For those experiencing significant hearing loss due to otosclerosis, surgical options such as stapedectomy or stapedotomy can offer remarkable advantages. During these surgical procedures, the fixed stapes bone is either removed or modified, and a prosthetic device is inserted, restoring critical sound transmission functions. The success rates for these surgeries are generally favorable, frequently leading to substantial improvements in hearing capabilities.
However, prospective candidates must carefully weigh the benefits against the inherent risks associated with surgical interventions, which may include complications such as infection or issues during the recovery phase. Consulting with a skilled otolaryngologist can assist individuals in making informed decisions, ensuring they have a clear understanding of the expected outcomes and potential risks before undergoing surgery. Surgical options can significantly enhance the quality of life for individuals grappling with severe hearing loss.
Considering Medical Management Strategies for Otosclerosis
While surgical interventions provide considerable benefits, medical management options such as fluoride therapy can also play a crucial role in the comprehensive treatment of otosclerosis. This particular treatment aims to decelerate the progression of the disease and is often considered for individuals who may not be suitable candidates for surgery or who prefer non-invasive alternatives.
Though the effectiveness of fluoride therapy remains a topic of ongoing discussion among healthcare professionals, there is evidence to suggest that it could benefit certain patients by reducing the rate of hearing loss progression. Regular monitoring and consultations with healthcare providers are essential to determine the appropriateness of this approach, ensuring that each individual’s treatment plan is personalized and effective in addressing their unique needs.
Understanding the Impact of Otosclerosis on Communication
Identifying Challenges in Conversations for Individuals with Otosclerosis
Engaging in conversations while dealing with otosclerosis can be an intricate challenge. As hearing loss advances, individuals may find it increasingly difficult to follow discussions, particularly in noisy environments where multiple sounds compete for attention. This struggle can lead to misunderstandings, frustration, and a sense of helplessness, ultimately affecting both personal and professional relationships.
The difficulty lies not solely in the ability to hear but also in maintaining meaningful connections. Conversations form the backbone of our social interactions, and when communication becomes strained, the repercussions can spread across various facets of life. Establishing a supportive environment—whether through compassionate friends and family or community initiatives—can help ease these challenges, promoting understanding and empathy for those living with otosclerosis.
Implementing Strategies to Enhance Communication
Utilizing effective communication strategies can significantly improve interactions for individuals living with otosclerosis. Employing visual cues, such as maintaining eye contact and observing facial expressions, can help bridge the gaps in understanding. Speaking clearly and at a moderate pace is crucial, as it enhances comprehension and facilitates smoother conversations.
Additionally, minimizing background noise in conversation settings can greatly contribute to successful interactions. Choosing quieter venues or utilizing assistive listening devices allows individuals to take proactive measures in creating a conducive communication environment. These strategies not only lead to clearer conversations but also reinforce the sense of community and connection among friends and family members.
Building Support Systems and Accessing Resources
Establishing a strong support network is vital for individuals navigating the complexities of otosclerosis. Support groups, whether in-person or online, provide invaluable spaces for sharing experiences and resources. Connecting with others who face similar challenges fosters a sense of belonging, enhancing emotional well-being and resilience.
Moreover, resources such as audiology clinics and advocacy organizations offer a wealth of information and tailored support for those living with hearing loss. From educational workshops to access to assistive technologies, these resources empower individuals to take charge of their auditory health while fostering connections within their communities. The strength found in shared experiences can illuminate the path forward for those grappling with the challenges of otosclerosis.
Exploring the Psychological Effects of Otosclerosis
Examining the Emotional Impact of Hearing Loss
The emotional consequences of otosclerosis can be deep and varied. As individuals confront the gradual loss of their hearing abilities, feelings of frustration, anxiety, and even depression may emerge, significantly affecting their mental health and overall quality of life. The burden of isolation can feel particularly heavy, especially when communication becomes strained and social interactions diminish.
Recognizing the emotional fallout is crucial for fostering resilience. Acknowledging these feelings and seeking help can lead to healthier coping mechanisms. Mental health professionals, along with supportive friends and family, play essential roles in guiding individuals through this emotional journey, helping them navigate the complexities of living with otosclerosis.
Developing Coping Mechanisms to Manage Emotional Challenges
For individuals grappling with the emotional challenges posed by otosclerosis, cultivating effective coping mechanisms can significantly enhance their overall quality of life. Counseling and therapy can provide valuable outlets for expressing feelings and exploring strategies for managing anxiety and frustration. Support groups amplify this process, creating a sense of community and shared understanding among participants.
Practices such as mindfulness meditation and journaling serve as effective tools for emotional regulation. These techniques promote a sense of calm and clarity, enabling individuals to process their experiences and adapt to the changes in their auditory landscape. Embracing these coping strategies can empower individuals to reclaim their emotional well-being and build resilience in the face of adversity.
Understanding the Impact of Otosclerosis on Relationships
The strain of hearing loss on relationships can be considerable, affecting communication dynamics and leading to misunderstandings between loved ones. It is essential for individuals with otosclerosis to communicate openly about their experiences, fostering an environment of understanding and support. Encouraging family and friends to ask questions and engage in discussions about the condition can promote empathy and strengthen connections.
Furthermore, involving partners and family members in the journey can enhance mutual understanding. Together, they can explore communication strategies and adapt their interactions to create a more inclusive atmosphere. By working collaboratively, individuals with otosclerosis can reinforce their relationships and navigate the challenges posed by hearing loss more effectively.
Preventive Measures and Lifestyle Adjustments for Otosclerosis
Implementing Preventive Strategies for Hearing Preservation
While otosclerosis itself cannot be prevented, adopting preventive strategies can effectively protect hearing from further deterioration. Safeguarding oneself from excessive noise exposure is paramount; wearing ear protection in loud environments, such as concerts or construction sites, can significantly reduce the risk of additional auditory damage.
Regular check-ups with audiologists are also critical for the early detection and management of hearing loss. By taking a proactive approach and staying informed about their auditory health, individuals can implement meaningful steps to preserve their hearing and mitigate the impact of otosclerosis on their lives.
Making Thoughtful Lifestyle Adjustments
Implementing mindful lifestyle adjustments can complement preventive strategies in addressing the challenges associated with otosclerosis. Adopting good ear hygiene practices, such as avoiding cotton swabs that can damage the ear canal, is essential for maintaining ear health. Additionally, fostering a balanced daily routine that incorporates regular exercise and healthy social interactions can contribute to overall well-being.
Establishing self-care routines—ensuring adequate rest and managing stress—can further support auditory health. By embracing a holistic approach, individuals can enhance their resilience and improve their capacity to cope with the effects of otosclerosis.
Adopting Nutritional Considerations for Ear Health
Supporting the body with a balanced diet rich in essential vitamins and minerals can play a crucial role in maintaining overall ear health. Nutrients such as vitamins A, C, E, and magnesium are known to contribute significantly to the preservation of the intricate structures found within the ear. Incorporating foods like leafy greens, nuts, and fish into daily meals can yield positive outcomes for those managing otosclerosis.
Consulting with nutritionists can provide personalized dietary recommendations, ensuring individuals receive the necessary nutrients to support their auditory health. By investing in a nutrient-rich diet, individuals may be able to slow the progression of otosclerosis while enhancing their overall lifestyle.
Utilizing Stress Management Techniques for Better Well-Being
The relationship between stress and otosclerosis is significant and should not be overlooked. High levels of stress can exacerbate symptoms, leading to increased anxiety and discomfort. Engaging in stress management techniques—such as mindfulness meditation, yoga, or deep breathing exercises—can be instrumental in alleviating tension and enhancing mental clarity.
Regularly practicing these techniques fosters a sense of calm, enabling individuals to better cope with the challenges associated with otosclerosis. Integrating relaxation practices into daily routines can lead to improved emotional well-being and a more resilient approach to managing hearing loss.
Frequently Asked Questions About Otosclerosis
What is otosclerosis and how does it affect hearing?
Otosclerosis is a condition that affects the middle ear, causing the stapes bone to become fixed, which results in hearing loss. It is often hereditary and primarily affects adults in their 20s and 30s.
How can I determine if I have otosclerosis?
Signs of otosclerosis include gradual hearing loss, tinnitus, and occasionally vertigo. If you experience these symptoms, it is advisable to consult an audiologist for testing and diagnosis.
What treatment options are available for otosclerosis?
Treatment options for otosclerosis include hearing aids, surgical interventions such as stapedectomy, and medical management options like fluoride therapy aimed at slowing disease progression.
Can otosclerosis be prevented in any way?
While otosclerosis itself cannot be prevented, protecting your hearing from excessive noise exposure and scheduling regular audiologist check-ups can help mitigate additional hearing loss.
How does otosclerosis impact daily living?
Otosclerosis can significantly affect communication and social interactions, leading to feelings of isolation and frustration if not properly managed.
What strategies can enhance communication for individuals with otosclerosis?
Employing visual cues, speaking clearly, minimizing background noise, and utilizing assistive listening devices can greatly improve communication for those living with otosclerosis.
What emotional effects are commonly experienced with otosclerosis?
Individuals with otosclerosis may experience feelings of frustration, anxiety, and depression due to the gradual loss of hearing, which can significantly affect their mental health and overall well-being.
How can I cope with the emotional challenges posed by otosclerosis?
Counseling, joining support groups, and engaging in mindfulness practices can help individuals manage the emotional challenges associated with living with otosclerosis.
What lifestyle changes can assist in managing otosclerosis?
Adopting preventive strategies, participating in regular exercise, maintaining a balanced diet, and implementing stress management techniques can be effective in managing the condition.
Are there specific dietary guidelines for those affected by otosclerosis?
A balanced diet rich in vitamins A, C, E, and magnesium can support overall ear health and may aid in slowing the progression of otosclerosis. Consulting with a nutritionist can provide tailored dietary advice.
Join us on our journey on X!
The post Otosclerosis and Its Impact on Hearing: An In-Depth Look appeared first on The Microsuction Ear Wax Removal Network.